ʻO ka pseudocyst Pancreatic: ka maʻi ʻana, ka mālama ʻana.
ʻO ka pancreatic pseudocyst (PC) kahi hui i hui ʻia no ka wai pancreatic i hoʻopuni ʻia e nā ʻōpala granula e noho ana a i ʻole a puni ka pancreas a hopena mai ka pancreatitis a pancreatic duct insufficiency. Hiki i nā Pseudocysts ke lilo a hoʻokahi a me ka lehulehu, ka nui a me ka liʻiliʻi, a hiki ke ulu i loko i waho a i waho o ka pancreas. ʻO ka hapa nui o ka pseudocysts e pili ana i ka papa pancreatic a loaʻa ka nui o nā enzyme digestive. Hōʻike ʻia nā paia o ka pseudocyst e nā ʻili kūleʻa e like me ka ʻōpū, ka koloka koloka, ligament gastrointestinal, a me ka pancreas. Hōʻike ʻia ka lihi o loko o ka PC e ka granule a me ka aʻa fibrous, ʻo ka haʻalele ʻana o ka lula epithelial e hoʻokaʻawale ana i ka PC mai ke kūkaʻi cystic maoli o ka pancreas.
Hiki i ke PC ke hele mai i 3 mau kūlana:
- Hiki i ka PC ke hoʻomohala ma hope o kahi hoʻouka ʻana o ka pancreatitis waha ma kahi o 10% o nā hihia 1.2. Hiki i nā necrosis o nā kiko peripancreatic ke hōʻea i ka nui o ka waiʻai me ka hui ma hope a me ka hoʻokumu ʻana i nā pseudocysts, hiki iā ia ke kamaʻilio me ke kumu o ka pancreatic. ʻO kahi kū'ē aʻe ke nānā aku i nā pseudocysts ma muli o ka nekrosis nui o ka parenchyma, hiki iā ia ke hana i ka hoʻopau piha ʻana o ka papa pancreatic me kahi kahe nui o ka wai pancreatic.
- Ma waena o nā mea maʻi me ka pancreatitis kūpaʻa, ʻoi aku ka nui o ka hopena o ka hōʻemi waiʻona, hiki ke hoʻokumu ʻia i ka PC ma o ka hōʻā ʻana o ka pancreatitis a i ʻole ka holomua ʻana o ka hana o ka papa pancreatic. Hiki i ke kīhāpai ke kūkulu i kahi hopena ma muli o ke ʻano paʻa o ka papa wai a i ʻole he ʻano kākuhi intraductal mai loko mai o nā plug protein. ʻO ka hoʻonui i ke kaomi intraductal hiki ke hōʻeha i ka leakage o ka wai pancreatic me ka hōʻiliʻili ʻana i nā ʻaha prepancreatic.
- ʻO kahi hōʻeha pōkole a komo i ka hōʻeha paha hiki i ka hōʻeha kino i ka umauma pancreatic i alakaʻi i ka hoʻokumu ʻia ʻana o kahi PC.
ʻO ka hapa nui o nā PC he asymptomatic, akā loaʻa paha iā lākou nā ʻano like ʻole o ka maʻi neʻe e pili ana i ka nui a me kahi i kau ʻia.
- Hiki i nā pseudocysts hoʻonui i ka ʻōpū ma ka ʻōpū, pale i ka duodenum, nā kīʻaha koko, a i ʻole nā mea hao ʻoi. ʻO nā fistulas me nā ʻōpala kokoke, hiki i ka pūpū pleural a i ʻole pericardium ke ʻano.
- Ka maʻi maʻamau me ke kūkulu ʻana o kahi kinona.
- ʻO ka hoʻoneʻe ʻana o nā moku pili i ke ʻano o ka hoʻokumu ʻana o pseudo-aneurysm, hiki ke hoʻoulu i ka nui o ka nui o ka nui a PK a i ʻole ke kahe mai ka gastrointestinal hopena ma muli o ke kahe ʻana i ka papa pancreatic.
- Hiki ke hoʻopiʻi ka puʻu a me ka pleurisy i ka wā i wāwahi ʻia ai ke kumu o ka pancreatic me ka hoʻokumu ʻana o kahi fistula me ka ʻōpū o ka ʻōpū a i ʻole ʻāʻī aiʻole i ka wā i haki ai ka PC.
Hoʻololi pinepine ʻia kahi maʻi PC me ka CT a i ka pāʻana. Ke hana nei i ka kahawai (ʻoi aku ka nui o ka therapeutic ma mua o nā kumu diagnostic), he ulu nui i ka pae amylase ma nā waihona PC, ma muli o kāna kamaʻilio ʻana me ka ʻōnaehana papa pancreatic, he ʻano o nā PC. ʻIke ʻia kahi kiʻekiʻe o ka amylase, ma mua o 1000, loaʻa i ka wai i loaʻa i ka hopena ma muli o ka laparocentesis a i ʻole thoracocentesis i nā pihi pancreatic a i ʻole pleurisy.
Nā hopena maʻi maʻamau
ʻO ka nīnau mua inā paha aia kekahi manawa e hōʻiliʻili ka ʻai i ka cystic neoplasm a i ʻole "pseudo-pseudocyst". Hoʻohana ʻia ʻo Cystic neoplasm e like me ka PC ke hōʻeha i nā hoʻopiʻi koʻikoʻi a hiki iā ia ke paʻakikī i ka hana ʻana ma hope. Pono nā ʻike i ʻike ʻia e hopohopo i ka hopohopo ʻo ke kūkulu ʻana i ka wai kaomi, ʻaʻole ia PC.
- ʻAʻohe mōʻaukala a i ʻole nā hōʻailona o ke aʻeha o ka pancreatitis a i ʻole a trauma.
- ʻO ka hala ʻole o nā loli hoʻololi pili i ka CT.
- ʻO ka heleʻana o kahi septa kūloko i loko o ka lua o ka cyst.
ʻOiai he kiʻekiʻe o ka amylase ma PC e pili ana i ka hui ʻana me ka pancreatic flow e hōʻike pinepine ana i kahi PC maʻi maʻi, e mau ana ke kiʻekiʻe kiʻekiʻe o ka kanalua ʻaʻole wale kekahi o nā hoʻokolohua wale nō e hiki ke haʻalele i ka cystic neoplasm. Pono nā maʻi ʻē aʻe ʻaʻole he lignant e hoʻohuli i ka PC, ma muli o kēia, pono loa ka mālama nui e pale aku i nā hemahema i ka hopena o ka 2.8.
Hiki paha ke hele mai o ka pseudo-aneurysm
ʻO ka nīnau hou e pili ana inā he pseudo-aneurysm, kahi hoʻopiʻi e loaʻa ana ma kahi o 10% o nā maʻi me PC 9-11. ʻO ka maʻi koʻikoʻi a hōʻeha paha ke ola ma hope o ka pauahi endoscopic inā ʻaʻole i manaʻo ʻia ka mea maʻi i ka pseudo-aneurysm. Inā ʻaʻole i hana embardization arterial i hana mua, a laila pseudo-aneurysm he contraindication koʻikoʻi i ka interoscopic intervent. ʻEkolu mau hōʻailona hōʻailona hōʻailona e hōʻike i ka hele ʻana o pseudo-aneurysm:
- ʻO ke kahe huehui a me ka ʻike ʻole.
- ʻO ka hoʻonui pinepine ʻia ma ka nui PC.
- Huli i loko o ka hematocrit.
Manaʻo mākou ua hana paʻa, bolus, ikaika scan CT ma ka imaging me ka hoʻomaʻamaʻa mua ʻana i ka arterial phase i lilo i papa hana maʻamau no nā poʻe maʻi āpau i manaʻo ʻia e nā poʻe moho no ka wai endoskopika e ʻike i ka pseudo-aneurysm. Maikaʻi paha kahi nānā Doppler o ka ʻōpū no ka ʻōpū, akā he haʻahaʻa haʻahaʻa. ʻO ka Angiography kahi hōʻailona wehewehe hoʻoweliweli a ke hoʻomau nei ia e hana no ka embolize pseudo-aneurysms me ka radiopaque spiral a i ʻole foam. Ma waena o nā mea maʻi 57 mua i ʻōlelo no ka hoʻōla ʻana o ka pseudocysts i kā mākou waihona, hiki iā mākou ke hoʻokuʻi i ka 5 pseudo-aneurysms ma mua o ka hana ʻana i ka kahawai. Ua mālama ʻia kēia mau mea maʻi ma o kahi ʻano multidisciplinary, me ka embolization a i ʻole haʻalele ʻia. ʻO ka mea hou loa, ua hana pono mākou i ka hoʻoheheʻe endoskopika ma hope o ka embolization ngiographic kūpono i nā maʻi nā maʻi ʻaʻole maikaʻi nā koho no ka huli ʻana.
ʻO ka hana o ka mālama conservative
Hoʻokumu ʻia ka hoʻomaʻamaʻa kuʻuna kuʻuna i ka hana papa ma ke ʻano papa haʻawina a nā PC e hōʻike nei ma mua o 6 mau heʻina i ʻike pinepine ʻia a, ma hope o ka nānā ʻana, hāʻawi i nā hoʻopiʻi ma ka 50% o nā hihia. Ma hope o 13 mau pule, ʻaʻole i ʻike hou ʻia a nui aʻe ka kiʻekiʻe o nā hoʻopiʻi. Ua noi ʻia e kaʻi ma hope o ka manawa no ka mālama he 6-pule e hōʻoia ai ʻaʻole i hele kū ʻia kahi kūʻokoʻa a hāʻawi i ka manawa e hoʻomaʻamaʻa ʻia ʻo nā pā o ka PC e ʻae i ka enterstomy cystic pololei e ke kuʻo. A ʻae ʻia kēia ʻano e nā lāʻau lapaʻau a maʻamau pinepine ʻo ia i hōʻike ʻia 15-18. Akā, ʻelua mau loiloi ʻē aʻe, e hōʻike aku nei i kahi hoʻokipa hoʻomohala a me ka ʻike hou loa i ka mea maʻi me ka loaʻa ʻole o ka cystic neoplasm, pseudo-aneurysm, a i ʻole ma mua o nā hōʻailona liʻiliʻi. ʻO ka loiloi retrospective o nā maʻi 68 me ka PC i mālama ʻia me ka conservatively i hōʻike ʻia i nā hōʻeha koʻikoʻi i ka 9% o nā hihia, ka hapanui o nā mea i hana i ka 8 mau pule ma hope o ke kūʻana. Hoʻokomo ʻia nā hoʻonāukiuki i ka hoʻokumu ʻana o ka pseudo-aneurysms ma 3x, perforation i loko o ka ʻōpū o ka ʻōpū manuahi i ka 2x a me ka hoʻomohala i ka hanana ʻole i ka mea maʻi 1st. Eia kekahi, ʻo 1/3 o nā mea maʻi e hana i ka hana koho mahele e pili ana i ka ʻeha e pili ana i nā cysts hoʻonui ʻia. Eia nō naʻe, ua hōʻike ka 43 mau mea maʻi (63%) i ka hopena a i ʻole ka loaʻa ʻana o nā hōʻailona a me nā hoʻopiʻi ma ka awelika e pili ana i nā mahina he 51. Ua nānā ʻia nā mea like like me kekahi 75 aʻoi aku nā maʻi maʻi. Ua hana ʻia ka hoʻokuʻi wale nō no ka ʻeha o ka ʻōpū o nā ʻōpū, nā hoʻopiʻi a me ka hoʻonui ʻana holomua nui o ka nui o ka cyst. 52% o nā mea maʻi e hana ʻia e like me nā mea i hōʻike ʻia ma luna nei, he ʻoluʻolu nā mea maʻi. I waena o nā mea maʻi o ka hui hope loa, 60% ka hoʻopau ʻana i ka hope o ka cyst a hiki i ka 1 makahiki, a hoʻokahi wale nō nā pilikia pū kekahi e pili ana iā PK. ʻAʻohe mau mea maʻi ʻē aʻe o kēia pūʻulu o nā hōʻailona i like ʻole, a i ʻole i ʻoki a hoʻonoho paha ʻo PK i ka nui. ʻAʻole hiki ke wānana, ma ke kumu o ka etiology a me CT, nā mea e hiki ai i nā mea maʻi i ka hoʻonā piha ʻana o PC. ʻAʻole i hāʻawi ʻia kahi wehewehe kikoʻī o ka anatomy o ke kumu o ka pancreatic, i hiki ke kōkua i ka wānana i ka hoʻomohala ʻana o ka maʻi mai ka ʻike ʻole ʻia.
Nā koho koho
I ka wā ma mua, ʻo ka waʻu e lilo i pono no ka hoʻopiʻi a i ʻole nā hopena ʻole e pili ana i ka PC, ʻo ke kaʻina holo ʻana ʻo ia wale nō ka mālama ʻana. I kēia manawa, ʻelua mau koho o ka mālamaʻana i lilo i mea kaulana: percutaneous a me endoscopic drainage. ʻO ke koena e kū nei i ke ʻano o ka ʻano o kēia mau hana e pono ai e hāʻawi ʻia i ka mea maʻi i kahi ʻano mua o ka ʻoihana. Aia i kēia mau ʻike hoʻohālikelike hoʻohālikelike o nā ʻelua hana, a hoʻohana nō nā kauka i ka mea a lākou e ʻike maikaʻi loa ai. ʻO ka hūnā ʻole o ka waikahe percutaneous o ka noho lōʻihi o ka catheter a me kahi mea hiki ke hoʻomohala ʻia kahi fistula o waho.
Holo palapala ʻauʻau. ʻO ka hapa nui, inā hiki, ke hoʻohana i ka kahe o ka wai o ka wai o loko, ka ʻano ʻānō e pili ana i ka localization o ka pseudocysts:
- Cysto-gastro a duodenostomy hoʻi i ke kūʻai ʻana i ka cyst me kahi ʻōpū a i ʻole duodenum.
- Hiki ke hoʻohana ʻia Cystejunostomy me nā koho anatomical ʻē aʻe.
- Hiki ke hoʻoneʻe ʻia ka huikiki pancreatic ma ka ʻae ʻana; ua pono pinepine ka papillosphincterotomy ma lalo o kēia mau kūlana.
ʻO ka nui o ka hōʻike o ka hoʻopiʻi ʻana i ka pāhaʻi wai loko e like me 15% me kahi maʻi make ma lalo o 5%. ʻO ka pae o ka hōʻemi postoperative e pili ana i ka 10% 22-26. Inā aia ka mākaʻi o ka papa nui o ka pancreatic ma lalo o ke kiʻekiʻe o ka anastomosis, makemake kekahi o nā kauka hou i ka haʻalele ʻana o ka PC, ma mua o ka alawai o loko i ka hoʻāʻo ʻana e hōʻemi i ka uku o ka hoʻi ʻana.
E pono paha ke ʻauʻau ʻokoʻa kūlohelohe waho inā hiki ʻole ke hoʻokumu ʻia kahi anastomosis kūloko. ʻO nā fistulas pancreatic ma waho ke hopena maʻamau o kēia ala.
Mahu ka papa kahawai. Hoʻomaʻamaʻa ʻia ke kahe wai Transdermal e like me ka hoʻokaʻawale ʻana i ka hakahaka ma loko o ka pānaʻi a me ka pani ʻana o nā cy sters a me ka maʻi i hoʻopaʻa ʻia ʻo 28-30. Pono e mālama pono i ka popoki o ka catheter e ka pale pono. Waiho ʻia ka catheter a hōʻemi ke kiʻekiʻe o ka hoʻokuʻu i ka 5-10 ml. i ka la. I loko o kahi noiʻi o nā mea maʻi he 52, ʻo ka nui o ka manawa hoʻolimalima wai 42. Inā ʻaʻole e hōʻemi ka mea like o ka neʻe i ka pae, a laila hiki i ke koho pono ʻana o ka octreotide (50-200 mg. Pono e nānā ʻia ka scan CT ma ke kaohi ʻana i ka nui o ka hoʻohemo i ka hōʻoia e hele ʻole mai ka catheter mai ka PC PC. ʻO ka hoʻopiʻi nui ʻana o kēia kaʻina hana ke komo ʻana ma o ka catheter o ka maʻi, i loko o kahi hōʻike hoʻokahi i hapa i ka hapalua o nā mea maʻi. ʻAʻole ʻike ʻia inā pono ka pale ʻana o ka papa pancreatic kumu nui loa e pale ʻia mai ka hana ʻana i ka wai a percutaneous.
Ke kaʻina hana Endoscopic. He nui nā hōʻike e hōʻoia i ke kiʻekiʻe o ka hiki o ka cysto-gastro endoscopic (ECG) a me ka cystic duodenostomy (ECD). ʻO ECD ke ʻano hana i koho ʻia ma muli o kona palekana palekana, ʻoi aku ka maikaʻi o ka hoʻoku ʻana ʻana i ka hopena i ka cyst i ka wā o ka kahawai, a me ka makemake nui ʻana i ka duodenum ma mua o ka ʻōpū i ka hapa nui o nā PC. ʻO ka pae hoʻonā o ke PC me ka mālama endoscopic ʻokoʻa mai ka 65 a 89%. ʻO nā maʻi koʻikoʻi nui o ka haki endoskopiko i ke kahe (ʻo ia, ma kāna hōʻeha, pono i ka hoʻomaʻamaʻi ʻana ke ʻano o ka 5% mau hihia), ka hoʻihoʻi retroperitoneal, ʻeha a me ka hiki ʻole ke hoʻonā i ka PC. ʻO ka make kino e pili ana i kēia kaʻina hana he hana kū ʻole me ka neʻe ʻana o ka 6-18%. ʻO ka nui o nā hihia o ka perforation a i ʻole koko ke hoʻemi ʻia e ka nānā ʻana i ka PC ma mua o ka puncture endoscopic. Maikaʻi mākou i ke nānā ʻana o PC ma ka puncture endoscopic, ʻoiai ke hoʻonui nei i ka mea kaulana o ka ultrasound endoscopic hiki ke hana i kēia ʻano i koho ʻia.
ʻO ke kuleana o ka ultrasound endoscopic
ʻO ka kaulana o ka ultrasound endoscopic i ka hopena o ka pseudocysts pancreatic e ulu nei i kēia manawa no ka meaʻo kēia ala hiki i kēia ʻano ke hiki iā ʻoe ke hoʻomaopopo i ka ʻano o ka hoʻopiʻi o ka pā a me nā mea i loaʻa o ka PC. I ka hui pū me ka biopsy aspire, hiki ke kōkua i ka hoʻoliʻoli ʻokoʻa ʻana o ka PC a me ka cystic neoplasm. ʻO ka hele ʻana o kahi septa ʻokoʻa, ka mucin echogenic, a me ka formum volumetric e hōʻike ana i ka neoplasm cystic e koi ana i ka ʻaihue a ʻaʻole hoʻoheheʻe ʻia. E like me ka mea i ʻōlelo ʻia ma luna nei, hiki i ka ultrasound endoskopiki ke kōkua i ke koho ʻana i kahi kahua puncture no ka pseudocysts - e kāpae i ka hele ʻana o nā veins nui a i ʻole nā ʻili i ke kula wai. No laila, i ka ʻepekema, loaʻa paha i kēia ʻano ke hōʻemi i ka hōʻemi o ke kahe a me ka hoʻokaʻa, ʻoiai ʻaʻole i hōʻike ʻia kēia i nā hoʻokolohua hoʻokolokolo.
ʻO ka heleʻana o ka necrosis pancreatic
Ke manaʻoʻiʻo nei mākou ʻo ka nīnau nui loa e pili ana i ka hoʻoholo e pili ana i ka hoʻohana ʻana i ka endoscopic, surgical a radiological drainage paha ʻo ia nō aia nā hōʻailona o ka PC pili me ka pancreatic necrosis, i hoʻoholo ʻia e CT me kahi ʻokoʻa ʻē aʻe. ʻO ka heleʻana o nā hōʻuluʻulu pōpilikia, dendrite, a me ka nānā ʻana i nā wahi o ka necrotic o ka parenchyma pancreatic e hōʻike nei he nui ka nui o ka nui o ka nui o ka mea i make. ʻO ka hoʻoholo e hoʻopili ai i ke ala kahe e pili ana i ka neʻe ʻana o ka nānā ʻana o ka necrosis. Hoʻokomo pinepine nā hoʻopiʻi hoʻopiʻi me ka hoʻohana ʻana i ka wai o endoscopic a me ka radiological i kēia mau kūlana. ʻOiai ʻo ka hapa nui o nā hoʻopiʻi i hōʻea mai ka puʻu endoskopiki hiki ke mālama ʻia i ka endoscopically e ka poʻe loea i ʻike ʻia, hiki ʻole ke hoʻomaopopo i ka necrosis, e hoʻopiʻi i ka hana wai ʻole / kōpili o ka fokus necrotic, hiki i nā hopena hoʻopiʻi nui a hiki i ka make. No laila, ʻo ka hele ʻana o ka necrosis pancreatic e pono e lilo i kumu nui loa no ke kanalua i ka hoʻokō ʻana o ka kanaki endoscopic, ʻoiai ʻaʻole ia e kāpae ʻia i kāna mau ho'āʻo ʻana. Hiki i ka hoʻomaʻamaʻa hoʻonāukiuki ke hoʻāʻo i ka PC ke hoʻoili i ka dendrite necrotic a loaʻa i ka holo mua ʻana o nā ʻike ma mua o ka hoʻopili ʻana o ka anastomosis. Hiki i kahi ala endoskopika me ka pīhoihoi transural e hiki ai i ka nasogastric lavage, hole dilatation me ka hoʻolauna ʻana i kekahi mau stents, a hiki ke lilo i kahi hana lapaʻau hou i nā maʻi maʻi i koho pono ʻia i nā kikowaena kūikawā. Hōʻike ʻia nā pilikia e kū nei ma kahi hōʻike o nā mea maʻi he 11 i loaʻa i ka wai endoskopika no kēia ʻano o ka cyst (wehewehe ʻia "ka maʻi pancreatic necrosis"). Ke hoʻohana nei i nā ʻenehana endoskopika wiwo ʻole, ua hoʻokō ʻia ka kūleʻa i 9 nā mea maʻi. Ua koi ʻia nā ʻano hana he nui me kahi helu hoʻopiʻi o ka 50%, ʻoiai ʻo ka hapanui o lākou ua mālama ʻia ma ka endoscopically.
Ke hōʻike nei i ka maʻi pancreatic
ʻO ka hōʻemi ʻana o ka pus i loko a i ʻole kokoke i ka pancreas ma ka ʻōlelo maʻamau ka mea i hōʻike ʻia e ka pseudocyst maʻi maʻi, kahi ʻano e koi koke ana i ka wehe a me ka huki.ʻO ka mea i hala koke nei, ua hoʻohana ʻia ka waika endoskopika i loko o kahi hui o nā maʻi me ka kiʻekiʻe o ka hoʻokō ʻia ʻana ma muli o ka hiki ʻana o nā ʻōnaehana hoʻopiʻi o ka pancreatitis. ʻO nā mea koʻikoʻi e lawa ka kahawai, ka pono pono e kāpae i ka huina o ka puka waho a me ke aʻo ikaika a me ka nānā ʻana i ka mea maʻi. Makemake mākou i kahi neʻe polokale e hoʻoheheʻe i ka kahe mai kahi mai hiki iā ia ke hoʻolako hou i ka waihā o ka kanawai cystenterostomy, ka hoʻokomo ʻana i kahi catheter irrigation nasogastric a me nā kumuono he nui e pale ai i nā pilikia i hoʻopili ʻia me ka haʻawina catheter a me nā mea i koe.
Mea Hoʻohui manaʻo
I kēia manawa, hoʻolaha mākou i nā hana hoʻomanawanui ikaika i nā maʻi me nā PC i hōʻea e like me ka hoʻopiʻi ʻana o ka maʻi a me ka maʻi pancreatitis me ka hele ʻana o nā hōʻailona a me ka lōʻihi o PC ma ka liʻiliʻi he 4 mau pule. Hana mākou i kahi HRCP inā noʻonoʻo mākou he mea maʻi ka mea maʻi no ka hoʻāʻo i ka hoʻomaʻamaʻa endoscopic. I ka wā o ka endoscopy, pono ke haʻalele ʻia ka portal hypertension a me ka haʻalele ʻana mai ka ʻōpū mai ka ʻōpū. Hana ʻia ʻo RCP e ʻike i nā hōʻailona o ka hoʻopiʻi ʻana i ka lāʻau biliary, ʻoi aku hoʻi i nā pihi hepatic i kiʻekiʻe. Pono ke pancreatography i nā maʻi āpau e hoʻomaopopo i ka lalo o ke ahulau papa pancreatic. ʻIke pinepine ʻia nā hana paʻa ʻole a me ka calculi o ka papa pancreatic i hoʻopaʻa ʻia, paʻa paha i ka maʻi maʻi ʻana e kū ʻia. No ka mea Hiki ke hoʻokō ʻia ka pālahalaha endoskopika ma o ka puncture punupua a me ka hoʻokūkū stent extra-papillary; nui loa ka pancreatogram no ka koho ʻana ma waena o kēia mau mea ʻelua. Hiki paha i ka ultrasound Endoscopic ka hopena ma ke ʻano maʻi maʻi me nā lesi pancreatic cystic a me ka hoʻoheheʻe ʻia o ka PC, ʻoiai ʻaʻole ia e hana maʻamau. ʻO nā maʻi me ka nunui, hoʻomau, a hoʻonui paha i nā PC e hōʻike pinepine i ka hōʻeha kino i ka hōʻeha ʻana i ka pancreatic, ka mea e hoʻoholo ai i ka pono a me ke ʻano o ka lāʻau lapaʻau i hoʻohana ʻia. I loko o ko mākou ʻike, hiki i ke kīpē o ka papa pancreatic a me kona paʻa pono ʻana i kēia pūʻulu o nā maʻi a ʻaʻole i hoʻoholo ʻia ma hope o ka hoʻonā ʻana i ka pseudocyst. Ke hoʻohālikelike nei, nā leakage mai nā lālā peripheral i pau ma hope o ka mālama ʻana ma ka endoskopika e alakaʻi i ka hoʻonā i ka cyst.
- Ma kā mākou hana maʻamau, hoʻomau mākou i ka mālama conservative, inā hiki, me kahi puʻuwai pancreatic kahi a hiki i ka huelo a me ka make ʻole o ka kamaʻilio me ka PC. Inā conservative ka mea maʻi, a laila hiki ke hoʻomalu ʻia ka nui o ka PC ma hope o ka manawa 3-6 mahina e CT o ka ʻōpū o ka ʻōpū. ʻO nā hōʻailona hou e like me ka ʻeha o ka ʻōpū, ke koʻo, a me ke kuni ka loiloi koke ʻia. E pono ke palekana i ka hoʻoheheʻe māmā ma lalo o kēia mau kūlana. ʻO ka fistula pancreatic kahi ʻano like ʻole. Eia nō naʻe, ʻo ka hemahema ua hoʻomau ʻia ka lawehala e ka catheter.
- Ke mālama nei i kahi puncture ma lalo o ka mana radiological e pono ke pale me ka nahu i ka duct, maha cysts a me nā nekrosis.
- ʻO kahi pseudocyst e pili pū ana me ka papa pancreatic, ʻoiai inā loaʻa kahi mamao loa mai ka paia o ka ʻōpū a i ʻole duodenum a ʻoi aku ka liʻiliʻi o 6 mm, ʻoi aku ka maikaʻi o ka hakahaka transpapillary.
- Hana ʻia ke kahe wai Transmural me ka papa holo piha o ka papa pancreatic a PC paha ka nui ma mua o 6 mm, kahi e hoʻonā ai i ka wā e hoʻohana ana i ka pāheʻe trans-capillary haʻahaʻa iki paha. Hiki ke mālama ʻia ʻo ka Endoscopic me ka lōkia kokoke i ka PC a me ka lumen i ka ʻōpū, i hoʻoholo ʻia e ka nui a me ka ultrasound endoscopic.
- ʻO ka hōʻeha koʻikoʻi i ka papa pancreatic e alakaʻi i ka hoʻopiha piha ʻana i ka huelo pancreatic i hiki ke pane i ka pāheʻe trans-capillary, ʻoiai e hana ʻia ka hoʻoheheʻe transally me kahi pū ka nui.
- Hiki ke hoʻohana ʻia kahi ala o ke ʻano leʻa me ka ʻūhā o ka lepo a i ʻole ka nui o ka wai o ka endoscopic a me ka pāheʻe.
Abstract o kahi ʻepekema ʻōlelo lāʻau i ka lāʻau a me ka mālama olakino, kākau ʻia o ka ʻepekema ʻepekema - Schastny A. T.
Hōʻike ka ʻatikala i nā pilikia o ka maʻi epidemiology, etiology, diagnosis a me ka mālama ʻana i nā pseudocysts o ka pancreas, hōʻike i ka hoʻonohonoho pono o ka maʻi. I hoʻoholo ʻia no ka polokalamu diagnostic no kēia pathology e hoʻohana i ka hoʻohana ʻana i ke ʻano noiʻi noiʻi ʻenehana hou (ultrasound, compute tomography, magnetic resonance imaging, cholangiopancreatography, endoscopic retrograde papillocholangiography, a me ka loiloi biochemical a me cytological o nā ʻike o ka cyst). Uku ka nānā nui ʻana i nā hana lapaʻau o ka hoʻomaʻamaʻa, inā hoʻi me nā ʻenehana minimally invasive. Hoʻokumu i ka ʻikepili palapala a me kā mākouʻike pono i ka mālama ʻana i nā mea maʻi 300, nā maikaʻi a me nā hemahema o nā ʻano like ʻole no kēia ala no ka ʻōlelo ʻana, ua kūkulu ʻia nā hōʻailona no ka mālama ʻana. Hōʻike ʻia i nā hana laparoscopic he ala hoʻohiki i ka mālama ʻana i nā mea maʻi me ka pancreatitis maʻi me ka pseudocysts.
Hōʻike ʻia nā nīnau o ka epidemiology, etiology, diagnostics a me ka mālama ʻana i nā pseudocysts o ka pancreas. Ua loaʻa i ka papahana diagnostic i kahi o kēia pathology e hāʻawi ʻo ia i ka hoʻohana ʻana o nā ʻano hana nui o ke ʻano o ka noiʻi (ʻimi ʻana iā ultrasound, kamepiula tomography, magneto resonant tomography, cholangiopancreatography, endoscopic retrograde papillocholangiography e like me ka biochemical a me ka analtological analima o ka ʻikā o ka cyst. Ua uku ʻia ka nānā pono ʻana o nā ʻano hana no ka mālama ʻana, ka mea nui hoʻi i nā ʻenehana mini-invasive.ʻO ka hoʻolilo ʻana i ka ʻikepili a me ka ʻike no 300 mau mea maʻi maʻi lapaʻau, nā pōmaikaʻi a me nā hemahema o nā pale umauma o ka hihia o kēia ala nāhelehele, nā hōʻailona no nā. ua hōʻike ʻia ka hana operative.Laparoscopies i hōʻike ʻia i kahi papa alakaʻi i loko o ka mālama ʻana i nā poʻe maʻi me ka maʻi pancreatitis paʻa me ka pseudocysts.
ʻO ka kikokikona o ka hana ʻepekema ma ke kumumanaʻo "Pseudocysts o ka pancreas: ka maʻi maʻi, ka mālama ʻana"
HELE NO KA AOAO NO NA HIKI HOA
ʻO nā pseudocysts o ka pancreas: Diagnosis,
UE "Vitebsk State Medical University", Regional Scientific a Practical Center "Hoʻomake ʻana i nā maʻi o ka ake a me ka pancreas",
Hōʻike ka ʻatikala i nā pilikia o ka maʻi epidemiology, etiology, diagnosis a me ka mālama ʻana i nā pseudocysts o ka pancreas, hōʻike i ka hoʻonohonoho pono o ka maʻi. I hoʻoholo ʻia no ka polokalamu diagnostic no kēia pathology e hoʻohana i ka hoʻohana ʻana i ke ʻano noiʻi noiʻi ʻenehana hou (ultrasound, compute tomography, magnetic resonance imaging, cholangiopancreatography, endoscopic retrograde papillocholangiography, a me ka loiloi biochemical a me cytological o nā ʻike o ka cyst). Uku ʻia ka nānā ʻana i nā hana ʻoi no ka mālama ʻana, ʻoi aku ka ʻenehana minimally invasive. Hoʻokumu i ka ʻikepili palapala a me kā mākouʻike pono i ka mālama ʻana i nā mea maʻi 300, nā maikaʻi a me nā hemahema o nā ʻano like ʻole no kēia ala no ka ʻōlelo ʻana, ua kūkulu ʻia nā hōʻailona no ka mālama ʻana. Hōʻike ʻia i nā hana laparoscopic he ala hoʻohiki i ka mālama ʻana i nā mea maʻi me ka pancreatitis maʻi me ka pseudocysts.
Nā huaʻōlelo: pancreas, pancreatitis, pseudocyst, surgery endoscopic
Hōʻike ʻia nā nīnau o ka epidemiology, etiology, diagnostics a me ka mālama ʻana i nā pseudocysts o ka pancreas. Ua loaʻa i ka papahana diagnostic i kahi o kēia pathology e hāʻawi ʻo ia i ka hoʻohana ʻana o nā ʻano hana nui o ke ʻano o ka noiʻi (ʻimi ʻana iā ultrasound, kamepiula tomography, magneto resonant tomography, cholangiopancreatography, endoscopic retrograde papillocholangiography e like me ka biochemical a me ka analtological analima o ka ʻikā o ka cyst. Ua uku ʻia ka nānā pono ʻana o nā ʻano hana no ka mālama ʻana, ka mea hoʻi i nā ʻenehana mini-invasive.ʻO ka hoʻolilo ʻana i ka ʻikepili a me ka ʻike no 300 mau mea maʻi maʻi lapaʻau, nā pōmaikaʻi a me nā hemahema o nā komo hewa o ka hihia o kēia ala nāhelehele, nā hōʻailona no ka operative ua hōʻike ʻia ka hoʻomaʻamaʻa.Laparoscopies i hōʻike ʻia i kahi papa aʻo i ka mālama ʻana i nā mea maʻi me ka pancreatitis maʻi me ka pseudocysts.
Huaʻōlelo: pancreas, pancreatitis, pseudocyst, mālama ʻana i ka pseudocysts, ka hana o ka endoscopic
ʻO nā cysti pancreatic no nā hui he nui a me nā ʻano like ʻole o nā maʻi pancreatic a he komohana o ka pancreatitis aʻehaʻeha a iʻole ke kaumaha. ʻO ke pinepine o ka hoʻomaka ʻana o nā pseudocysts ma nā papa pancreatitis maʻa a me nā maʻi ʻo kēia maʻi hoʻi i hoʻopaʻa ʻia i loko o kahi nui o nā noiʻi. Pili
ʻO ka hapa nui o nā pseudocysts hilinaʻi i nā ala diagnostic. ʻO ka pancreatitis enakī he paʻakikī e kahi cyst i 5-19.4% o nā hihia, ma nā hana koʻikoʻi o ka pancreatitis luku kino - a i kahi 50% o nā hihia. I ka hihia o ka hōʻeha ʻana o ka pancreatic, hele mai nā cyst i 20-30% o nā mea hōʻeha, a me nā pancreatic pseudocysts i loko o ke ʻano o nā hoʻopiʻi o ka maʻi pancreatitis maʻi e hele ana i 20-40% o nā hihia. Hoʻohana ʻē aʻe
Ua hōʻike ʻia nā hopena ʻo ka pancreatitis hoʻonaninani maʻamau ma mua o ka hoʻomohala ʻana o ka pseudocyst pancreatic i loko o 56-70% o nā maʻi. Eia kekahi, ma 6-36% o nā hihia, ʻike ʻia nā cyst me ka pancreatitis biliary, 3-8% ma hope o ka hōʻemi kino ʻana a i ʻole hōʻeha, a ma 6-20%, ʻaʻole i ʻike ʻia ko lākou kumu. Hiki i ka Pseudocysts ke hoʻonui iā lākou iho i nā hōʻeha huhū (ka huhū, ka ʻeuʻeu, ka ʻōpū), e ulu ana i 25% o nā maʻi. ʻOiai ka hoʻomaikaʻi ʻana i nā hana lapaʻau, ʻo ka hoʻokomo ʻana i nā ʻano o ke ʻano o ka mālama koʻikoʻi ma ka hoʻomaʻamaʻa ʻana, ka make ma ke kōnuhā ʻana o ka pancreatic he 27-42%, a inā he sepsis, koko, a me ka hoʻonaninani ua hiki aku i ka 40-60% 2, 3.
I kēia manawa, loaʻa ka nui o ka ulu ʻana o ka maʻi hōʻino a me ka pancreatitis paʻa, a ma muli o ka hoʻomaikaʻi ʻana a me ka wā i hoʻonui ʻia ʻo nā ʻano loiloi diagnostic hou, ke ʻano nui o ka pseudocysts nui. Pono nā hana loiloi a me ke koho o ke ʻano lapaʻau ke kumuhana o ka kūkā. No laila, ke kūleʻa nei ka ʻimi no ka hiki ʻana i ke kaʻina holoʻokoʻa no ka pancreatic cysts, e pili ana i kā lākou etiology, localization, ka pilina me ka papa hana pancreatic, a me ka hiki ʻana o nā hoʻopiʻi. Hāʻawi ʻia i kēia, ʻo nā pilikia o ka lāʻau lapaʻau no ka maʻi pancreatic e koi hou i ka noiʻi ʻana i ke kūkulu ʻana i nā taktika kūpono loa a koho i kahi wawaʻi kūloko, kahi i hoʻoholo ai i ka pili o kēia pilikia.
E like me ka ʻōlelo a M. Calley a me W. Meyers e hui pū nei me ka manaʻo o nā loea he nui, "Surgical
"hoʻomau ka paʻamau i ka mālama ʻana i nā hōʻailona a me ka hoʻopiʻi o ka hōʻuluʻulu ʻana o nā huaʻaloa o ka wai o ka wai, pancreatic pseudocysts a me ka pohihihi." Hoʻokumu ʻia nā hana hoʻolālā loiloi ma ke kumu o ka ʻano o ka maʻi, kahi, ma ke ʻano, i hōʻike ʻia e M. Sarner. " e pane i nā nīnau ʻekolu, he aha ka hewa? he aha i hana he aha e hiki ai? Ua manaʻo ʻia kekahi mau papa inoa o nā pseudocysts pancreatic.
Ka hoʻokaʻawale ʻana i ke ʻano inoa ma Atlanta i ʻehā mau ʻano like ʻole o ke kaʻina pili.
1) kahi hōʻiliʻili wili o ka wai i ka wā mua o ka pancreatitis o ka maʻi me ka pohō i ka paia o ka granulomatous a i ʻole nā mea kiko o ka palu,
2) pseudocysts kūpuka - kahi lua i hoʻopuni ʻia e ka iwi fibrous a granulomatous paha, he hopena ia o ka pancreatitis a i ʻole trauma,
3) pseudocysts mau hopena i hopena mai ka maʻi pancreatitis a me kahi neʻe ʻole ma mua o kahi hanana o ka pancreatitis o ka maʻi,
4) pancreatic abscess, intra-abdominal hōʻemi o ka pus ma ke kokoke o ka pancreas me a ʻole ʻole necrosis e hopena ana i ka maʻi aʻeha paha a kahi maʻi trauma.
Kahi ʻōnaehana papa inoa, i hāpai ʻia i ka makahiki 1991 e A. DʻEgidio a me M. Schein, ua hoʻokumu ʻia a nānā i ka helu a me ka pae o ka kamaʻilio ʻana o ka ʻōnaehana pancreatic me ka pseudocyst cavity
1) iʻa kūpaʻa i ke kua o kahi loli maʻamau pancreatic,
2) nā pūniki e kū mai ana i ke ʻano o ka maʻi pancreatitis me nā leka protocococystic pinepine, akā me nā wili ʻole ma ke kumu o ka pancreatic dute.
3) pūnohu maʻamau i hui pū me nā
nā loli nui i ka papa pancreatic nui, ma keʻano like, me nā hana paʻa ma ke kumu o ka pancreatic main.
ʻO W. Nealon a me E. Walser ka papahele ʻana i ka pseudocysts pancreatic e like me ke duct anatomy a me ka hele a ʻaʻole i pilina me ka lua o ka pseudocyst. ʻO ke kumu o kēia helu, ʻo ka hoʻolana ʻana i nā loina maʻamau no ka mālama kūpono ʻana i ka pseudocysts pancreatic.
ʻO ka algorithm diagnostic o pseudocysts pancreatic e pili ana i ka hoʻohanaʻana i ka ultrasound, composible tomography, magnetic resonance imaging, cholangiopancreatography, endoscopic retrograde papillocholangiography a me ka nānā ʻana i nā ʻike o nā cyst biochemically a me cytologically. Wahi a ka helu helu Atlantean, kahi ʻano pseudocyst e ka hele ʻana o ka paia o ka pā o fibrous a granulomatous, aʻo kahi hōʻuluʻulu ʻili o ka wai o ka ʻaʻole. Akā ke hele nei i nā hōʻailona o ka suppuration, nā ʻāpana o ka nekrosis, ka mea e hoʻoponopono ai i nā loiloi morphological e ʻike ʻole ʻia, no laila, e pili ana ka maʻi ma ke ʻano o ke kauka o ka mea maʻi 9, 10.
ʻO kēia mau kaʻina hana diagnostic, ʻo ka ultrasound ke kūpono loa, ka uku a me ka invasive. Pono e hoʻopaʻa ʻia kēia haʻawina ma ke ʻano he hana mua i ka hoʻomohala ʻana o nā cysts pancreatic. ʻO ka ʻike diagnostic o ke ʻano ʻo 88-100% a ʻo ka mea kikoʻī ʻo 92-100%, akā ʻo ka hopena he hilinaʻi nui loa ia i ka ʻike a me nā hōʻailona o ke kauka. Ma lalo o ka hoʻomalu o ka ultrasound, hoʻomaʻamaʻa nā punctures o nā hana cystic me ka hoʻokolokolo o hope o nā manaʻo, akā naʻe, a
Kuhi. 1. Ui. Kūmole pancreatic
invasive pamamaraan, pono e hoʻohana i dopplerography kahi'ōlau e ike kiʻi i nā kahe koko ma ke kokoke i ka pseudocyst a i kona pā.
Manaʻo ia ʻo ka compute tomography he papa noiau ma ke ʻano o ka pseudocysts. Hiki ke koho iā ʻoe e koho i ka wahi o nā pseudocysts, ka mānoanoa o kona pā, ka hele ʻana o ka necrosis, sequesters, septa, a me ka ratio o nā pseudocysts i nā koko koko i loko o ka foci. Loaʻa ka tomography hoʻohālikelike - 82-100%, kikoʻī - 98% a me ka pololei - 88-94% 11, 12.
ʻO kekahi o nā hana noiʻi koʻikoʻi ʻo retrograde pancreatic
Kuhi. 2. KT. Puku kaila pihi.
Kuhi. 3. Retrograde virsungografiya.
cholangiography (RPCH). Hāʻawi ʻo RPHG i ka ʻike pili i ke anatomy o ka pancreatic a me nā kēne bile a kōkua i ka hoʻonohonoho ʻana i nā pseudocysts pancreatic. ʻOiai hāʻawi ʻo RPCH i ka liʻiliʻi o ka ʻike e pili ana i ka nui o nā cyst, kona wahi, puni nā kiko, ka pilina o ka pseudocyst me ka pancreatic duct paha
Kuhi. 4. MRPHG. Puku kaila pihi.
ua ʻike ʻia ma 40-69% a me kēia, hiki ke hoʻololi i nā ʻatikala o ka mālama ʻana, no ka laʻana, e hoʻohana i ka waʻa transpapillary. Ua hōʻike ʻia nā haʻawina ma 62-80% o nā mea maʻi he retrograde e hoʻopiha ana i ka pseudocyst me ka hoʻohālikelike ʻana, ʻo ia hoʻi, ua hōʻoia ʻia ka pilina o ka pū me ka pancreatic duct. ʻO kahi mea nui hoʻi kahi mea i hōʻike ʻia e nā maʻi pancreatic duct, ʻo ia ke kumu o ka hoʻomohala ʻana i ka pseudocysts. Ma ka huli ʻana, ʻo ka retrograde ka hoʻohālikelike ʻia o nā papa o ka bile a me nā kēla pancreatic hiki ke alakaʻi i nā hoʻopiʻi koʻikoʻi, e like me ka cholangitis, pancreatitis, a me ka maʻi o ka cyst.
I kēia manawa, ʻoi aku ka nui o ka magnetter resonance pancreatocholangiography (MRPC) i makemake nui ʻia. ʻAʻole hoʻohiki ke ʻano, a me ka haʻahaʻa hoʻopiʻi haʻahaʻa haʻahaʻa ma mua o RPHG, a hilinaʻi nui ʻia hoʻi i nā ʻoihana loiloi ma mua o ka ultrasound, a me ka ʻike o MRPC he 70-92%. Nui nā mea kākau o MRPC i kapa ʻia ʻo "standard standard" o ka noiʻi a manaʻoʻiʻo e hiki ana i ka wā e hiki mai ana, me ka hoʻomohala ʻana o ka ʻenehana MRI, e hoʻohuli ke ʻano o ke ʻano hana i loko o nā hana kūwaho.
ʻO ka hana nui o ka mālama conservative i loko o nā mea maʻi me ka pseudocysts he haʻahaʻa loa, haʻahaʻa loa 2, 14, 15. Nui nā mea lapaʻau e hilinaʻi nei i ka hoʻonui ʻana o nā cysts ma lalo o ke kumu o nā anti-inflammatory therapy, akā he mea ʻoi loa kēia no ka hōʻemi nui ʻana o ka wai maʻi i loko o nā mea maʻi ma muli o ka maʻi pancreatitis 2, 16.
S. McNees et al. ʻike ʻia he hapa ma mua o ka hapalua o nā mauhele pankreʻehā e paʻapū i ka paʻakū
i ku i ka olelo. No laila me ke ʻano o ka nui o nā kahe wai e hōʻiliʻili ʻia (e like me nā ʻōmaʻomaʻo a me ka noi ʻana o KT), me ka nānā ʻana i ka ʻeha a i ʻole nā hōʻailona o ka hoʻouluulu ʻana i nā ʻūpiki o ka hapanui e ka ulu ʻana o ka hoʻomoʻe wai. Aia ka hopena o ka hoʻonā spontan maʻamau o ka cyst mai 8% a 85%, e like me ka etiology, kahi a me ka mea nui loa, ma ka nui o ka pseudocyst. Ma waho o ka hoʻomaʻamaʻa ʻana, hiki i nā pseudocysts ke nalowale i nā manawa i loko o nā hebedoma 46 ma hope o kahi hanana o ka pancreatitis aʻokiʻoki. I ka pancreatitis kūlohelohe, maʻamau nui ka hopena o ka cyst ma muli o ka pā i hoʻopuni piha ʻia, me ka ʻokoʻa ʻole o nā hihia i loaʻa ʻole i ko lākou haki ʻana i ka ʻōpū a i ʻole ka lolo dile 18, 19, 20. E like me A. Warshaw a me D. Rattner, he pseudocyst hiki ʻole ke hoʻoholo like ʻole.
- ina he mau pule ko ka 6 mau pule,
- me ka maʻi maʻamau,
- i mua i kahi aniani a i ʻole ka paʻakikī o ka wai pancreatic (me kaʻole o ke kamaʻilioʻana me ka pseudocyst),
- inā a puni ka pseudocyst e kahi pā uhi.
E like me ka mea i hōʻike ʻia ma luna, ua hoʻoholo ʻia ka hiki ke hoʻōla pono ʻia e ka nui o nā pseudocysts: ʻo nā cysts i nunui ma mua o 6 cm ua aneane ʻaʻole loa e hoʻopau ʻia me ka pale ʻana, a, e like me kekahi mau hōʻike, ʻo ka pseudocysts nui loa a 4 cm e loaʻa ana i ka extrapancreatically e hoʻomau i ka ulu ʻana o ka haukapila me ka hoʻomohala ʻana o nā hoʻopiʻi.
Таким образом, случаи регресса и «самоизлечения» сформированных панкреатических кист не могут рассматриваться как повод для пассивной тактики их лечения . Необходимо учитывать, что панкреатические псевдокисты, как указывалось, часто осложняются нагноением, перфорацией в свободную брюшную полость, реже плевральную, а также кровотечениями в
cystic cavity a i loko o ka lumen o ka gastrointestinal tract. ʻO ke ʻano o ka hana ʻana i nā hana hōʻeuʻeu kūpū e kūʻē i ke kua o kahi hoʻopiʻi kūlohelohe nui i ʻoi aku ka paʻakikī, a ʻoi loa ka paʻakikī. Eia nō kekahi, ʻo ka ʻōhaka cystic o ka pancreas hiki iā ia ke hoʻololi i kahi maʻi cystic a i ʻole cyst me ka hōʻino.
E like me ka hapa nui o nā mea kākau 6, 18, 22, 23, he mau hōʻailona no ka pale ʻana i ka pseudocysts i ka:
ʻO ka hoʻopiʻi o kahi pseudo-cyst (hoʻokahi mākeke ua lawa):
- ka hooneʻe ʻana i nā moku nui (i ʻole a i ʻole iā ka ʻōlelo ʻo CT),
- stenosis o ka ʻōpū a i ʻole duodenum,
- keena kūwaho o ka umauma bile,
- kahe koko ma ka pseudocyst,
Nā hōʻailona o ka pseudocyst pancreatic:
- nausea a luaʻi,
- kahe ʻana mai ka gastrointestinal mokulele kiʻekiʻe.
Asymptomatic pancreatic pseudo-cysts:
- pseudocysts ʻoi aku ma mua o 5 cm, ʻaʻole e loli i ka nui a mau aku i nā wiki 6.
- ka laula ma mua o 4 cm, aia kahi extrapancreatically i loko o nā mea maʻi me ka maʻi pancreatitis o ka etiology alkoholā,
- ka manaʻo o ka hōʻino.
Ke loaʻa nei nā ʻōkuhi no ka lapaʻau ʻana, ua hoʻokokoke aku mākou i nā nīnau koʻikoʻi i lalo: he aha nā ala o ka hana
radios a ma kahi e pono ai e hoʻohana no ka pseudocysts a me nā hōʻuluʻulu nui o ka wai leʻa, he aha ke ʻano o ke koho - e hana ana i ka hanana kūmole a puʻuwai minimally invasive surgery? I kahi ākea ākea, ka hopena o ka wawa aku nei e ka pae ʻana o ka ʻokoʻa ʻana o ka maʻi o ka pseudocyst pancreatic a me kona mau paia. ʻOi aku ka nui o ka cyst a me kona paia, ʻoi aku ka nui o nā manawa ma laila e hana i ka ʻona radical 2, 24, 25. Akā, ʻo ka lōʻihi o ka noho ʻana o ka cyst he paʻakikī i ka hoʻoholo ʻana, a me nā mea kū hou e paʻakikī ana ke wānana i ka hoʻomohala ʻana i ka hoʻopiʻi a me ka pilina me ka system ductal. I kēia hihia, hāʻawi ʻia kahi wahi nui i ka hoʻokō ʻana o nā hana hoʻokele minimally invasive ma ke ʻano he ʻano hoʻōla a ʻo ia paha. Nui nā ʻano o ka puncture, catheterization i hana ʻia ma lalo o ka mana o ka ultrasound a me ka tomography computed, a me ka laparoscopic interventions, i kēia manawa he nui nā mea kākoʻo a ua manaʻo ʻia he mea hou o nā hana kuʻuna kahiko 1, 26. Eia nō naʻe, i ko mākou manaʻo, e noʻonoʻo pono nā ʻano o ka laparotomy kūlohelohe hana.
ʻOiai ka hoʻomohala ʻana o nā ʻenehana minimally invasive a me ka hoʻomohala hou o ka CT a me ka ultrasound, ʻo ka hana mau ka mea nui no ka mālama ʻana i nā mea maʻi me ka pancreatic pseudocysts 27, 28, 29.
Hoʻokomo ʻia ka hoʻomaʻemaʻe ʻana i ka loiloi kūloko a me waho. Ua hōʻike ʻia ke ala o ka hana maʻi i ka mea maʻi: a) me ka pseudocysts paʻakikī, ʻo ia hoʻi, ka maʻi a me ka necrotic, b) me nā pseudocysts e pili ana i ka hoʻopaʻa ʻole ʻana a i ka hoʻoneʻe ʻana o ka auhau, c) me ka neoplasia cystic i hopohopo, d) me ka hui pū ʻana o ka pseudocyst a me ka stileosis bile. mau ala, e) me nā hoʻopiʻi, e like me ka pīhoihoi ʻana o ka ʻōpū a i ʻole duodenum, perforation
walkie-talkie a me ke koko no ka hiolo ʻana o nā ʻalihi a i ʻole pseudo-aneurysms. Mālama ʻia ka manawa o ka hana ma ka hiki ʻana o ka pā cyst. I ka pancreatitis kūlohelohe, hiki ke lawelawe ʻia i ka pseudocysts me ka ʻole o ke kali iki, e like me ka manaʻo i ka wā o ka make ʻana o ka pā cyst ua hana ʻia a hiki ʻole ke pale aku i nā ʻōlapa, ʻoiai ʻo ka wā mākaukau loa no ka pseudocyst e ʻoi aku ka paʻakikī 1, 20.
Hōʻike ʻia ka hika o waho no nā cysts immature me nā mea i hoʻopili ʻia a no nā puʻuwai pahū. ʻAʻole pili kēia i pili i nā maʻi me ka maʻi pancreatitis maʻi, ke ʻole ka hoʻomohala ʻana o ka pankī pancreatic ma hope o ka hoʻoili ʻana i ka hoʻouka kaua ʻana o ka pancreatitis o ka mea make. Ke manaʻoʻiʻo ʻia nei nā hōʻike ʻana no ka kaomi o waho o nā pūnoho pancreatic i loaʻa i ka 25-30% o nā mea maʻi me ka supuration a me ka hele ʻana o ka sequestration lehulehu i loko o ka lua. ʻO kekahi o nā hemahema nui o ia mau hana ʻo ia ka hopena kiʻekiʻe o ka hoʻomohala ʻana o nā papa pancreatic waho a me nā kūlana maʻamau. Hiki i ka lōʻihi o kēia mau hōʻeha ke kau i ka 10-30% 2, 19.
ʻO ke kahe o loko o ke ala o ke koho no nā pseudocysts maikaʻi uncomplicated. Aia i ka anatomy topographic, hiki i ka pseudocystogastrotomy ke kūpono no nā cysts kokoke i ka pā posterior o ka ʻōpū. ʻO nā liʻiliʻi (15 cm) nā cysts, kūpono no pseudocyst-unostomy. Aia i ka hoʻohālikelike ʻana paha e like nā hopena o ka pseudocystogastrostomy a me ka pseudocystoduodenostomy. ʻO Pseudo-cystogastrostomy ka mea i maʻalahi i ka maʻalahi, ka wikiwiki, a me ka liʻiliʻi o ka hoʻonāukiuki i nā hoʻopiʻi.
ka hana ʻoi, akā e pili pinepine ana i ke koko gastrointestinal pinepine mai ka gastrointestinal tract kiʻekiʻe. E ʻike nui ʻia ka kaulana o Pseudo-cystejunostomy, a ʻoi aku ka maikaʻi o nā hopena ma mua o ka pseudocystogastrostomy. K. Newell et al. ʻAʻole wau i ʻike nui i ka nui o nā cyst relapses a mortally ma waena o cystogastro a me cysto-unostomy, akā ua liʻiliʻi ka lōʻihi o ka hana a me ke koko ma hope o cystogastrostomy.
ʻO kahi contraindication pili i ka hana o ka paila o loko o ka maʻi o ka pūpono, kahi kaʻino i hana ʻia i ka pancreas, ke kahe ana i loko o ka lua o ka pūpoki a i duodenum, a me kahi pahu o ka pūpana i hana ʻole ʻia. ʻO ka hoʻohana nui ʻana o ka anastomoses cystodigestive i hoʻopaʻa ʻia e ka pilikia o ka hoʻomohala ʻana i nā hoʻopiʻi postoperative: nele o ka sastures aastomotic, exacerbation o ka pancreatitis, ka hoʻopiʻi arrosive. I ka wā o ka wā postoperative, inā paha me nā pseudocysts me nā hōʻailona o ka mumū, ulu ka edema anastomotic, e alakaʻi ana i ka hopena o ka wahiʻu me ka hoʻomohala ʻana i ka insolvency a i ʻole ka hoʻomaha ʻana o ka cyst i ka wā e hiki mai ana, no laila, aia nā manaʻo e hoʻohui i ka noi ʻana o ka anastomosis me nā koho ʻē aʻe no ka luawai o waho.
ʻO ka pale aku kahi hana hou no ka paewa o loko i loko o ka pseudocysts maʻi a me nā hōʻailona no ia mea: ka pancreatitis kūlohelohe, ka nui o nā cysts, gastrointestinal i hoʻokahe ʻia mai nā pseudoaneurysms, kahi o ka pile dile maʻamau a i ʻole duodenum, a me ka hiki ʻole e hoʻoheheʻe ʻia ka pseudocyst. Hana ʻia nā ʻōkiʻi ʻana i nā ʻano ala like, me ka ʻaoʻao o ka ʻaoʻao hema a me ka pancreatectomy ʻūlū hema
ʻO Pipple, pancreaticoduodenectomy me ka mālama ʻana i ka pylorus, ʻo ka mea iā Beger a i ʻole Frey). Hoʻokuʻu ʻia ka hōʻemi ʻana i ke kino a me ka lālani o ka pancreas me ka cyst no nā cysts i loaʻa i ka hapalua mamao o ka pancreas, no nā keaka lehulehu, no ka mea hoʻopiʻi hewa ʻana o ka cyst, a no nā mea maʻi me ka relapses ma hope o ke kahe ʻana o ka cyst (Fig. 5, see color insert). Distal pancreatic resection alakaʻi i ka nalowale ʻana o kahi hapa nui o ke kumuhana, i hiki ke hoʻonāukiuki i ka hoʻomohala ʻana o ka maʻi mellitus a i ʻole ka pancreatic insufficiency.
Hiki i ka hana o ke cystectomy ke hana i loko o nā nānā i hoʻokahi me ka pseudocysts liʻiliʻi i loaʻa. O ka paʻakikī o ka hana ʻana, ʻo ia ka pono e hoʻokaʻawale i ka paia o ka pseudocyst mai nā ʻaoʻao kokoke a i ka pūpū o ka pancreas.
E noʻonoʻo i nā mea hiki ke hoʻopihapiha. A hiki iā lākou ke hoʻololi i keʻano kūlohelohe? He aha nā hōʻiliʻili minimally i komo paʻa i ka lāʻau kaua o ka mea maʻi i ka mālama ʻana i ka pancreatitis maʻi a me nā mea hoʻonā?
ʻO kekahi o nā ala no ka Endomopiko pancreatic decompression ʻo ka endoscopic papillotomy a wirsungotomy me ka endoscopic drainage 32, 33. ʻO ka pahuhopu ke hana i ka pilina ma waena o ka lua pseudocyst a me ka gastrointestinal tract. ʻO nā koho ʻē aʻe no ka hoʻokumu ʻana i ka anastomosis ua loaʻa i ka transpapillary a i ʻole transmurally. Inā kamaʻilio ka cyst me ke kumu ʻo ka pancreatic, a laila lilo ka wai transpapillary i ke ʻano o ka koho. Ua hana mua ʻia ka sphincterotomy a me ka cannulation ma o ke kaʻe o ka lua o ka cyst, a laila ma ke kumu
ua waiho ʻia he poli waiho 19, 34. Me nā hōʻailona o ka manaʻo o ka cyst, ka hele ʻana o nā masa necrotic, kahi hoʻohui pū kahi i hoʻohui ʻia i loko o ka lua o ka cyst ma ka ihu no ka moʻo a me ka holoi ʻana. I ka awelika, e like me ka poʻe kākau mea, ʻo ka stent a hiki i ka 4.4 mau mahina (me ka lāe o ka cyst), a me ka hoʻololi ʻana no ka stent ma hope o nā wiki 6-8, 35, 36, 37. pancreatic duct hypertension. Eia nō naʻe, he mau ʻōlelo hoʻopiʻi ka transpapillary, e like me ka neʻe ʻana a ka hopena ma nā wahi mamao a me ke ākea, exacerbation o ka pancreatitis, ʻae ʻana o ka stent a, ma muli o ia, o ka hoʻohemo ʻana o ka paho. Ua hōʻike ʻia nā haʻawina ʻo ka loaʻa ʻana o ka stent obliteration ma 50% o nā mea maʻi i 6 mau pule ma hope o ka hoʻokomo. Aia nā lono e pili ana i ka holomua o nā loli o ka pathological i ka pancreas a me nā keʻena me ka lōʻihi. Ma hope aku, mai 8-26% o nā mea maʻi e hoʻokele nei i ka hana ʻana ma ka hoʻohana ʻana i ke ʻano kuʻuna 25, 34.
Hoʻohana ʻia ka hakahaka transmural me kahi pseudocyst nona ka paia e pili kokoke i ka paia o ka ʻōpū a i ʻole ka duodenum, a i ʻole ka peʻa hoʻi ko lākou pā. Hōʻike ʻia ka ʻonaʻawae ʻokoʻa e ka tomography compute, ultrasound a ʻimi paha loiloi endoskopika, kahi i ʻikea ai ka wahi o ka cystic bulging i loko o ka lumen o nā mea maʻi. Ma o kahi endoscope, puncture o ka cyst a me ka minamina o nā ʻike, a laila ka puka i loko o ka paia o ka ʻōpū a me ka cyst e hana ʻia me kahi pū kaila. Hoʻowalewale ʻia ka lua o ka pūʻai e kahi catheter, kahi i hoʻokaʻawale ʻia ma hope o ka pau ʻole o ka cyst. Hiki iā ʻoe ke hana i ka pīhoihoi transpapillary a i ʻole hoʻoheheʻe wai i ka hihia o 92% a me 100%.
teas, kēlā me 37, 39.
ʻO nā mea ʻino loa a me nā maʻi koʻikoʻi o ka hoʻoheheʻe waila e hoʻoheheʻe nui ʻia mai ka paia o ka ʻōpū a i ʻole duodenum. Pono lākou i ka hoʻokō ʻana. Kuhi ʻia ka nui o nā pōpilikia o ka ʻōpū a me ka hoʻoheheʻe ʻole ʻana ma kahi kī 9, 26, 37. Kuhi ʻia kahi punahele ma hope o ka hoka o ka pseudocyst mai ka 66% a 81%. Ke hoʻopaʻa nei i nā ʻōlelo like ʻole e pili ana i ka hoʻohana ʻana i ka wai o endoskopika, hiki ke ʻano ʻia nā ʻano aʻe e hana ai no ko lākou hoʻokō 6, 10, 19, 39:
1. ʻO ka mamao mai ka pseudocyst a i ka paia o ka digestive tract ka mea ma mua o 1 cm.
2. Hiki i ke komo o ke kiʻekiʻe convexity o pseudocysts i ka pā kokoke.
3. Ka nui i oi aku ma mua o 5 cm, pēpē o ka ʻōpū, hoʻokahi cyst, kahi e pili pū ana me ka papa pancreatic,
4. Pōpio maikaʻi, inā hiki ma mua o ke komo transpapillary, e hana ana i ka pancreatography,
5. Screening no ka oki ʻana i kahi pseudocyst,
6. ʻO ka hemahema o ka mālama ʻana i ka mālama ʻana, ʻoi aku ka lōʻihi o nā maʻi ma mua o 4 hebedoma,
7. E haʻalele ʻole ʻo Neoplasm a me pseudo-aneurysm.
Wahi a E. Rosso, nāna i hana i ka loiloi o ka hakahaka o ka pualudocyst o ka pseudocysts o nā transmural a me transpapillary ma nā maʻi 466, ua loaʻa ka helu hoʻopiʻi ka 13,3%, ka pihoihoi o ka cyst a ua mālama ʻia e ka hoʻomaʻemaʻe ʻana i ka hoʻomaʻemaʻe.
ʻO ka hōʻiliʻili o ka pseudocysts, hōʻiliʻili nui o nā wai kūlohelohe, nā cysts akene ma lalo o ke kaohi o ka ultrasound a i ʻole ʻo CT kekahi wahi o ka mālama ʻana i manaʻo ʻia he mea hou no ka hana kuʻuna. A inā he endoskopika
No ka mea ʻaʻole i hoʻohana pinepine ʻia i loko o nā hale lapaʻau o ko mākou ʻāina, nā mea maʻi a me nā kaʻina hana maʻi ma lalo o ka mālama ʻana i ka ultrasound i paʻa i loko o ka waihona lāʻau o nā lāʻau lapaʻau i nā ʻoihana lehulehu. Hoʻopiʻi ka pāheu Percutaneous i kahi o waho o ka catheter, lawe ʻia ka wai kahe ma o ka mea lawe 7-12 B "ʻoi ʻia ka puaʻa" a i waiho ʻia nā pū wai 14 - 16 B. Hoʻopili ʻia ka waʻu ma kahi trocar kūikawā. Eia kekahi, aia nā koho pono no ka hoʻoheheʻe ʻana ma o ka ʻōpū, ma o ka duodenum, ka transhepatic, transperitoneal a me retroperitoneal. Hoʻomaopopo kekahi o nā hiʻohiʻona maʻamau i ka hoʻohana ʻana i ka launa wai percutaneous. No laila, e like me kekahi mau mea kākau, ʻo ka lōʻihi o ka hoʻohana ʻana i ka catheter (ʻoi aku ma mua o 6-7 mau pule) e alakaʻi i ka hana ʻole o ke ʻano ma ka 16% o nā hihia, hoʻohemo i ka 7% o nā hihia, a hiki i ka nui o nā hoʻopiʻi e hiki ke 18%. ʻO kekahi mea nui nui, ʻo ia ka nele o ka ʻano o ka pānaʻi transdermal i loko o nā poʻe maʻi me ka maʻi pancreatitis, ʻoi aku ka pili o ka pseudocysts me ka ʻōnaehana wai 3, 7. Wahi a ka ʻike o K Helee e! a1. , ua loaʻa ka hopena maikaʻi ʻaʻole i loaʻa pinepine i ka 42% o ka nānā ʻana, akā i ka manaʻo o b. Oi11o, i nā mea maʻi me ka pancreatitis kūpaʻa, aia nā pseudocysts i hoʻoneʻe ʻia a me nā wahi holo wai. He nui nā mea kākau e hoʻololi i ke kaʻina hana hoʻoheheʻe me ka punle pono-pulima ponoi me ka manaʻo o nā puna cyst, e pale ai i nā hoʻopiʻi i pili pū ʻia me ka catheter, ʻo ia ka maʻi, catheter occlusion, hoʻololi ʻia ka ʻili o ke kino i ka wahi wai. ʻO nā hōʻeha hōʻeha ka hoʻokomo ʻana i ka leakage o ke kahawai a i ʻole ka wehe ʻana i ka catheter me nā ʻike o ka pseudocyst e komo ana i ka ʻōpū o ka pūhaka. ʻOiai ke kauoha
ʻO kēia mau hoʻonālikelike, ke ʻano o ka puncture percutaneous a me ka hoʻoheheʻeʻana o ka pseudocyst ma kahi hopena o ke kūmole pancreatitis e hiki ke noʻonoʻo i ke kaʻina koho i kēia manawa.
ʻO ka wehe ʻana i ka laparoscopic no ka pseudocysts hiki nō ke hoʻopili ʻia i ke kuhikuhi o ka hana hōʻokiʻī minimally 41, 42. Ka ʻike me ka laparoscopic cystogastrostomy a me ka pseudocystejunostomy i kaupalena ʻia. ʻEkolu mau ʻano o ka nui o ka ʻano laparoscopic kūloko o ka puna wai i loko: ua intramural cystogastrostomy, aima cystogastrostomy a me ka posterior cystogastrostomy 13, 18. Ua hoʻohana pinepine ʻia nā ʻaoʻao ʻelua. I ka hihia mua, ua hoʻokomo ʻia nā trocars i ka lumen o ka ʻōpū a ua ʻoki ʻia ka paia posterior me kahi coagulator, i ukali ʻia e ka hoʻokumu o ka anastomosis. Me ka cystogastrostomy mua, hana ʻia kahi gastrotomy a he ʻano hanana anastomosis ma o ka paia o ka pā o ka ʻōpū. Ke hoʻohana nei nā lua ʻelua i nā stapler, akā ua kūʻai pinepine ʻia ka cystejunostomy a he nui nā hōʻike e pili ana i ka maikaʻi o ka palapala. ʻO ka pono o ka laparoscopic interventions ka hoʻoponopono hou a me ka noho hoʻomaha pōkole. Kuhi pū nā mea noiʻi i nā hoʻopiʻi o kēia ʻano: exacerbation o ka pancreatitis, kahe koko mai ka anastomotic zone. I loko o ka haukapila, ʻo kēlā me nā hōʻiliʻili o nā mea maʻi, ʻoiaʻiʻo, e koi aku i nā kikowaena kūikawā, nā lako kiʻekiʻe a me nā mea hana. Ke hōʻuluʻulu nei i ka noi o nā hōʻemi minimally invasive i loko o ka hana honua, pono e hoʻomaopopo ʻia ʻoiai ua hōʻuluʻulu ʻia ka ʻike nui, ʻaʻole naʻe nā ʻikepili i nā hopena lōʻihi (ʻoi aku ka pae o ka laparoscopic), he mau hua hopena hoʻohālikelike o nā ʻano lāʻau lapaʻau a me nā hanana lapaʻau kahiko.
ical hana. Eia nō naʻe, ke hana nei nā ho'āʻo e hoʻoholike i nā hana, hoʻomohala i nā hōʻike, a me nā contraindications. No laila i nā protocols o ka American Society of Gastroin-Testinal Endoscopy, ke hōʻike nei nā ʻākala i lalo.
1. I kēia manawa, ʻaʻohe mau ala kūpono o ka mālama ʻana i nā mea maʻi me nā neoplasms cystic, ka hoʻolele ʻana o ka endoskopika punahele ʻo ka pancreatic cysts me nā ʻokoʻa wale nō ke ʻano o ke ʻano o nā mākeke.
2. Pono ʻia kahi scan ultrasound.
ʻO ia ia, ʻo nā mea nui o ka "makaʻala" a me ka loaʻa o nā mīkini kiʻekiʻe.Heluhelu kekahi mau mea kākau i nā hōʻike hōʻike e hōʻike nei no ka hana ʻana i nā kuʻuna kuʻuna 6, 8, 15, 19:
1) ka nānā ʻana o nā contraindications i ka hoʻohana ʻana o nā hana endoscopic a i ʻole ka radiological a i ʻole ka ʻike ʻana i ko lākou hiki ʻole ʻana.
2) ka hui pū ʻana o kahi pseudocyst me nā hana paʻa o ka pancreatic d
3) i nā māla paʻakikī, no ka laʻana, ka hui pū ʻana o kahi pseudocyst me kahi "maʻi maʻi" i ke poʻo o ka pancreas,
4) ka hui pū ʻana o kahi pseudocyst me ka paʻa o ka dile bile maʻamau,
5) hui pū kekahi o nā hakahaka anuu,
6) mau pseudo-cy,
7) localization o ka pseudocyst i ka hu o ka pancreas,
8) ke koko i hoʻomāo ʻole ʻia e ka embolization,
9) kānalua i ka ʻano o ka cyst.
Ma kēia nānā ʻana i nā hana minimally invasive o ka mālamaʻana i ka maʻi pancreatitis i kaupalena ʻia e nā hiʻohiʻona o ka anatomy o ke pancreas a me ka pancreatitis.
puʻuwai, ke kiʻekiʻe o kā lākou loli. Ke hōʻike nei i nā hana kūpono o ka ʻōnaehana wai, ka pilina o ka pseudocyst me nā kumu wai, hiki paha i nā mea ke hoʻohana i nā hana lapaʻau maʻamau mai ka hoʻomaka mai 8, 15, 19.
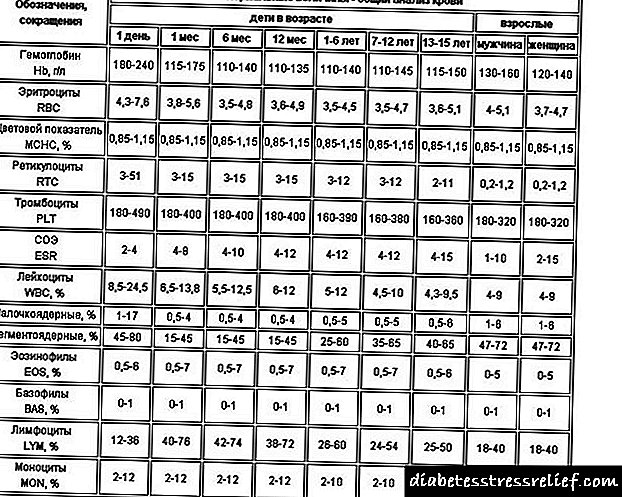
I kēia manawa, loaʻa iā mākou kekahi meaʻike pono me ka hoʻohana ʻana i nā nui o ka nui o nā kaila i luna no ka pseudocysts. 300 nā mea maʻi me ka pancreatitis kūpaʻa me ka noho ʻana o pseudocysts i lawelawe ʻia ma ka Vitebsk Regional Scientific a Practical Center "Hana ʻana i nā maʻi o ka Hōʻī a me Pancreas". ʻO ka ʻikepili ma ke ʻano o nā ʻano hana a kekahi mau hopena i hōʻike ʻia i ka papaʻaina.
ʻO kahi kikoʻī kikoʻī o kā mākou mau huahana pono aku ma mua o ke kāʻei o kēia ʻatikala;
E like me ka ʻike ʻana mai ka papaʻaina, hoʻohana mākou i kahi pālahalaha ākea ākea. Ma ka holoʻokoʻa, ka nui o nā hana kahawai (49.7%). Ua hoʻohana ʻia nā hana hoʻohālikelike i ka 24.7% o nā hihia, a me nā hōʻemi hōʻemi hōʻemi minamina ma 24.3%. E like me nā ʻōkuhi ma nā hui like ʻole, ʻo ka hapa liʻiliʻi o lākou he mau inoa i hoʻohana ʻia me nā ʻenehana minimally invasive. Eia naʻe, pono e ʻōlelo e pili ana i ka pohō me ka pseudocyst puncture ma lalo o ka mana o ka ultrasound i hoʻomaʻamaʻa nui ʻia ma ke ʻano a me kekahi manawa i hiki ʻole ke hoʻokaʻawale i nā papa pancreatic a me nā ʻano o nā hana i hana kūʻē ʻia i ke kūpaʻa o nā hoʻopiʻi o nā cysts (ka pehu, ka ʻaihue). I ka manawa like, loaʻa ole laparoscopic drainage surgeries (cystogastro- a me ka cystejunostomy) ʻaʻohe mea e hoʻopiʻi ai, ka mea i hōʻole ʻia i ka pono o ka ʻōlelo. He ʻokoʻa nā hoʻopiʻi postoperative i ko lākou hoʻolālā. ʻO ka helu nui, he postoperative
ʻO ke ʻano o nā mea hoʻoponopono hoʻokō ʻia me pseudocysts a me kā lākou
Nā Hoʻopau Maemae Abs. n, abs.
Ke hoʻolauleʻa 149 (49.7%) 27 18.12 6 4.03
1. Cystogastrostomy + puka kahe o waho
2. Duodeiocystovirsung ostomy 12 2 16.67
3. Du de n o qi waiwai 41 6 14.63 1 2.44
4, Cystogastrostomy 33 7 21.21 2 6.06
5. Cystejunostomy 26 3 11.54 I 3.85
6. Pakreatocis! ʻO nā poʻohiwi a ʻo wau ʻo 8 12.5
7. Pancreatogastrostoma 2
8. Kahe makahaa 24 8 33.33 2 8.33
9. Cystomentopexy me ka papa lepo o waho 2
Haimoku 74 (24.7%) 12 14.86 1 1.35
1. Hoʻokaʻawale i ka pancreatic hema a me ka cyst 38 3 5.26 1 2.63
2. Hoʻomoe ākea ʻo ke poʻo pancreatic (Begei ') 26 8 30.77
3. Ka hoʻihoʻi mua ʻana o ke poʻo pancreas (version Bernese) 5 I 20
4. Hoʻokele ʻele. 5
Hoʻopili hōʻeha iki nā minimally 73 (24.3%) 3 4.11
1. Laparoscopic cystoejunostomy 8
2. ʻO ka cystogastrostomy Laparoscopic 2
3. Puncture a me ka huki ma lalo o ke kaona ultrasound 62 3 4.84
4. Kālā lipi Laparoscopic 1
I. Kuehu 4
TOTAL 300 42 14 7 2.33
mea hana a me nā mea hoʻopiʻi - 15 nā mea maʻi, ke koko - 7 nā maʻi maʻi, fistula pancreatic - 9 nā mea maʻi, ka make suture - 4 nā maʻi maʻi, fistula biliary - 3 nā mea maʻi, a me ka pylephlebitis hoʻokahi-nānā, thromboembolism, kahi e hoʻopuka i ka ʻōpū, ka coagulation nekrosis o ka hau anuanu.
Ke hōʻuluʻulu i nā moʻolelo a me ko mākouʻike ponoʻī, ʻae mākou iā mākou iho e kiʻi i kekahi mau manaʻo a hāʻawi i nā ʻōlelo aʻoaʻo i ka mālama ʻana i nā pseudocysts.
I ko mākou manaʻo, ʻoi aku ka maikaʻi o ka mālama ʻana i nā maʻi me nā cysts e puka mai me ka liʻiliʻi
ʻenehana kikowaena. Hoʻomaopopo ʻia ka Puncture a me nā huki e hoʻopili me kahi hoʻonui o ka nui o ka cyst, ka hiʻohiʻona o ka ʻeha a i ʻole ka hoʻomoʻi ʻana o nā mea pili kokoke. I kā mākou nānāʻana, me ka hoʻokumu ʻana o nā cysts, ka wawa a ma lalo o ka kaohi o ka ultrasound i kōkua ai e ho'ōla i ka kokoke o 70% o nā maʻi, ka mea hoʻohālikelike ʻia me nā ʻikepili o nā mea kākau haole.
ʻO ka mea pono o ka kahawai percutaneous o ka pseudocysts i ka pancreatitis maʻi he kanalua. Aia i loko o ia mau kūlana e pono ke ʻano o ka pae ʻana o ka maʻi i ka haʻalele a hōʻoia i ke kaʻina kūloko, noiʻi
nā ʻike o ka cyst, e hōʻike ana i ka pili o ka cyst me ka ʻōnaehana ductal.
Hiki ke hoʻohana ʻia nā ʻenehana endoskopika (hoʻoheheʻe transway a me transpapillary) i nā mea maʻi i pili i ka pōkole me ka pā o ka ʻōpū a i ʻole duodenum a i ʻole nā pilina ma waena o ka cyst a me ka ʻōnaehana wai ʻO ka mea pōʻino, ʻo ka nele o kā mākou noiʻi ponoʻī i ʻae ʻia i kahi loiloi piha o kēia mau hana.
Manaʻo ka luawai o waho o ka pseudocyst he mea kūpono ʻole no ka lika ʻana o ka pā cyst me ka hoʻomohala ʻana o ka peritonitis a i ʻole ka maʻi o ka pūpona e kū'ē nei i kahiʻano o ke kūlana koʻikoʻi o ka mea maʻi.
ʻO ka honu i loko o ka hana kaila o ke koho no ka mālama ʻana i nā pseudocysts uncomplicated. Wahi a ka localization a topographic anatomy, cystogastrostomy, cystoduodenostomy, a i ʻole cystoejunostomy e pono e hoʻohana ʻia. ʻAʻole kūpono kēia ʻano hana i nā mea maʻi me ka pancreatitis capitate a i nā hihia kahi i hoʻopau ʻole ai ka anastomosis i hoʻokumu ʻia. ʻO nā koho no ka luawai o loko, ke koho maikaʻi loa, ma ko mākou manaʻo, ʻo ka cystoeunostomy, mai ka mea me ke kīwī o ka ʻōpū i huli ʻia ma hope o ka Ru, hiki i ka anastomosis ke kūkulu ʻia i kahi kokoke o kēlā me kēia wahi o ka pūlani, a me ka nānā ʻana i ka mōʻaukala o kona pā. ʻO Cystejunostomy, hoʻopili ʻia e ka hoʻoheheʻe ʻia o ka lua o nā cyst, e hoʻohana no nā cysts i hoʻopilikia ʻia.
ʻO nā ala o ka pale ʻana, ʻoiai me ka paʻakikī o kā lākou hoʻokō, he radical i ka mālama ʻana o nā mea maʻi me ka pseudocysts, eia naʻe, i ka wā e hana ai i kēia ʻano hana, pono ia e hoʻoikaika no ka mālama nui loa i ka hopena o ka endo- and exocrine pancreatic function, no ka mea alakaʻi lākou i ka holoʻana o ke kō
maikaʻiʻole beta aiʻole pancreatic.
Hoʻohana ʻia ka haʻalele ʻokoʻa no ka cysts i ka lōʻihi o ka hapalua o ka pancreas, no ka nui o ke keʻena a me nā keʻena hopohopo, a me ke kuhi ʻia ʻana ma hope o ka kahawai. Me ka pseudocysts me ke kūloko i ke poʻo o ka pancreas, pono ia i ka helu mua i ka helu ʻana i nā loli o ke poʻo o ke pancreas, ka mea i kapa ʻia "ʻōpala ākea". I nā mea maʻi me ka pancreatitis kūpaʻa me ka pseudocysts a me ka hoʻopiʻi concomitant o ka bile duct a me duodenum, ka hoʻokokoke o ka proximal e hōʻike ʻia (Kausch-Whipple surgery, pyloric-mālama i PDR a duodenum-mālama i ka pale o ka pancreatic). I loko o ka pancreatitis kūlohelohe, pono e kuhikuhi ʻia ka hana e hoʻopau i ke "ʻenehana hōʻeha", ʻo ia ke poʻo i hoʻololi ʻia ka pancreas. Hoʻomoe ʻo Proximal (Operation Beger) a i kāna "Bernese version" hoʻopau i nā ʻeha ʻeha a me kēia mau hōʻeha. Hāʻawi ʻia kēia koho o ka hana hōʻiliʻili i ka mea maʻi me ke koko i ka lua cyst a me ka hoʻokumu ʻana o pseudo-aneurysm.
Manaʻo mākou i nā hana laparoscopic ma ke ʻano he alakaʻi hoʻohiki i ka mālama ʻana i nā mea maʻi me ka pancreatitis maʻi me ka pseudocysts. I ka manawa like, makemake wau e hoʻomaopopo he pono loa e koho ke koho i nā mea maʻi no kēia mau hōʻuluʻulu, e noʻonoʻo ana i nā contraindications i luna.
Ke hoʻopau nei i ka hōʻike ʻana o ke kumuhana ma lalo o ka kūkā ʻana, manaʻo mākou he mea pono e haʻi iā Ch. Russell: "He mea nui ke koʻikoʻi ʻo ka mālama ʻana i nā cysts ʻaʻole hiki ke hoʻopau i ka pilikia o ka maʻi pancreatitis. No laila, e hoʻohui i nā hana no kahi cyst i kahi loiloi piha o
ka pancreas holoʻokoʻa a me ke kūpaʻa ʻana i ka nīnau inā he i a i ʻole he koʻikoʻi ka papa o ka pancreatic. "
1. He lokomaikai, P. A. ʻO ka hoʻokele hou ʻana o nā pseudocysts pancreatic / P. A. Grace R. C. Williamson // Br. J. Surg. - 1993. - Vol. 80. - P. 573-581.
2. Danilov, M. V. Pancreatic kaʻina / M. V. Danilov, V. D. Fedorov. - M .: Kauhane, 1995 .-- 509 p.
3. Usatoff V. Ka hana maʻi o ka pseudocysts i nā mea maʻi me ka maʻi pancreatitis / V. Usatoff, R. Brancatisano, R. C. Williamson // Br. J. Surg. -2000. - Vol. 87. - P. 1494-1499.
4. Callery, M. Ka mālama maʻi lapaʻau o nā pseudocysts ma hope o ka pancreatitis maʻa / M. Callery, C. Meyer // ʻO ka pancreas / ed. H. Beger et al .. - Berlin: Blackwell Science, 1998 .-- P. 614-626
5. Sarner, M. Ka papa helu ʻana o ka pancreatitis / M. Sarner, P. B. Cotton // Gut. - 1984. - Vol. 25. - P. 756-759.
6. Bradley, E. L. A ʻōnaehana helu maʻi lapaʻau e pili ana i ka maʻi pancreatitis / E. L. Bradley // Arch. Nā mea hoʻohālikelike. - 1993. - Vol. 128. - P. 586-590.
7. DʻEgidio, A. Pancreatic pseudocysts: kahi papa kuhikuhi i koho ʻia a me nā ʻano hoʻokele waiwai nona / A. DʻEgidio, M. Schein // Br. J. Surg. - 1991. - Vol. 78. - P. 981-984.
8. Nealon, W. hoʻokele hoʻomalu o nā hoʻopiʻi e pili ana i ka percutaneous a me / a me ka hoʻokele endoskopika o ka pseudocyst o nā pancreas / W. Nealon, E. Walser // Ann. Nā mea hoʻohālikelike. - 2005. - Vol. 241, N 6. - P. 948-960.
9. Loaʻa nā hopena ma hope o ka hoka o ka endoscopic no ka pankudis pancreatic, ka pseudocyst pancreatic aʻai, a me nā pseudocysts pancreatic maʻi / T. H. Baron et al. // Gastrointest. Endosc. - 2002. - Vol. 56. - P. 7-17.
10. Lehman, G. A. Pseudocysts / G. A. Lehman // Gastrointest. Endosc. - 1999. -Vol. 49, N 3. - Pt. 2. - P. S81-S84.
11. Hawes, R. H. Mana hoʻokō o ka pseudocysts / R. H. Hawes // Rev. Gastroenterol. Hōkeo - 2003. - Vol. 3. - P. 135-141.
12. Hoʻomoʻa ʻana i ka pancreatic e ka ultrasound a me ka tomography compute: kahi loiloi laulā / J. K. Lee et al. // Radiol. Kauaka. Akau. - 1979. - Vol. 17. - P. 105117.
13. Sugawa, C. Endoscopic retrograde pancreato-graphy i ka hoʻokō ʻana o ka pancreatic pseudocysts / C. Sugawa, A. J. Walt // Surgery. - 1979. - Vol. 86. -P. 639-647.
14. Beger, H. G. Duodenum mālama mālama i ke poʻo o ka pancreas i loko o ka maʻi pancreatitis koʻikoʻi:
nā hopena mua a me nā hopena hope loa / H. G. Beger, M. Buchler, R. R. Bittner // Ann. Nā mea hoʻohālikelike. - 1989. - Vol. 209, N 3. -P. 273-278.
15. Russell, C. Nā hōʻailona no ka hana / C. Russell // ʻO ka pancreas / ed. H. Beger et al .. - Berlin: Blackwell Science, 1998 .-- P. 815-823.
16. ʻO ka pilina o Porutaneus o ka pseudocysts pancreatic e pili ana me ka ʻoi aku ka nui o ka loaʻa ʻole ʻana ma mua o ka loaʻa ʻana o nā maʻi maʻi i hoʻopaʻa ʻole ʻia o ka maʻi / R. Heider et al. // Ann. Nā mea hoʻohālikelike. - 1999. - Vol. 229. - P. 781-787. - Haka. 787-789.
17. McNees, S. Percutaneous Management of Pancreatic Collections / S. McNees, E. van Sonnenberg, B. Goodarce // Ko nā pancreas / H. Beger et al .. - Blackwell Science, 1998. - Vol. 1, N 64. -P. 650-655.
18. ʻO nā mea wānana i ka hopena o ka pseudocysts e hoʻopiʻi nei i ka maʻi pancreatitis maʻi waiʻona /
B. Gouyon et al. // Kekahi. - 1997. - Vol. 41. - P. 821825.
19. ʻO ka pseudocyst pancreatic i ka pancreatitis kūlohelohe: endoskopika a me nā mea lapaʻau lapaʻau / E. Rosso et al. // ʻ .lelo. Nā mea hoʻohālikelike. - 2003. - Vol. 20. - P. 397-406.
20. Warshaw, A. L. Imi wa wai o ka hōʻeha wai no ka pseudocyst pancreatic. Nā lāʻau lapaʻau a me nā ʻoihana kūlohelohe / A. L. Warshaw, D. W. Rattner // Ann. Nā mea hoʻohālikelike. - 1985. -Vol. 202. - P. 720-724.
21. Waclawiczek, H. W. Der Schutz der pankreaticodigestiven Anastomose nach Pankreaskopfresektion durch Pankreasgangocmissions mit Fibrin (Kleber) / H. W. Waclawiczek, D. Lorenz / / Chirurg. - 1989. - N 6. - Bd. 60. - P. S403-S409.
22. Izbicki, J. R. ʻO ka hoʻopiʻi ʻana o nā ʻōpū pili i pili i ka maʻi pancreatitis e mālama ʻia ana e ka mālama duodenum mālama i ke poʻo o ka pancreas / J. R. Izbicki,
C. Bloechle, W. T. Knoefel // Br. J. Surg. 1994. Vol. 81. - P. 1351-1355.
23. ʻO Ridder G. J. Kūpono punahele o ka cystadeno-over adenocarcinoma o ka pancreas ma hope o ka curative resection / G. J. Ridder // V Eur. J. Surg. Oncol. -1996. - Vol. 22. - P. 232-236.
24. Gullo, L. Pancreatic cysts: somatostatin a me ka huki / L. Gullo // Cronic pancreatitis / ed. M. Buechler et al .. - Heidelberg: Blackwell pub., 2002. - P. 467-470.
25. Pākuʻi wai transpapillary Endoscopic: kahi hana a me nā hopena / R. Venu et al. // Gastrointestinal Endoscopy. - 2000. - Vol. 51, N 4. -P. 391-395.
26. Ka hoʻokele ʻana i ka pancreatitis akene: mai ka hana ʻana i ka mālama interventional intensiveional / J. Werner et al. // Kekahi. - 2005. - Vol. 54. - P. 426-436.
27. ʻO nā mea hoʻonāukiuki i loko o ka maʻi pancreatitis / E. I. Halperin a me nā mea ʻē aʻe // ʻO ka hōʻuluʻulu pancreatic ma ka manawa o ke kenekulia: mau mea Ros.-German. ʻōpūtou. - M., 2000 .-- S. 38-39.
28. Grishin, I.N. Hana maʻi pancreatic / I.N. Grishin, G.I. Askaldovich, I.P. Madorsky. - Mn .: Ke kula kiʻekiʻe, 1993. - 180 p.
29. Leonovich, S. I. Diagnosis a me ka mālama ʻana o ka maʻi pancreatitis i kākau ʻia: kākau ʻia. . ^ E Ha yM. dis. Kauka med. Nā ʻepekema: 14.00.27 / S.I. Leonovich. - Mn., 1995 .-- 33 p.
30. Kaopuahi, A. M. Kaohi kulana o na pnu pseudocysts pancreatic / A. M. Cooperman // Surg. Kauaka. Akau Am. - 2001. - Vol. 81. - P. 411-419.
31. ʻO cystgastrostomy ka cystjejunostomy a me nā hana e pili ana i ka pseudocysts pancreatic? / K. A. Newell et al. // Hoʻokele. - 1990. - Vol. 108. -P. 635-639. - Haka. 639-640.
32. Pākuʻi papa ʻo Endoscopic a me ka noho ʻana no ka pancreitis a me ka pancreatic cyst a me ka ʻauamo / N. Shinozuka et al. // J. Hepatobiliary Pancreat. Nā mea hoʻohālikelike. - 2007. - Vol. 14, N 6. - P. 569-574.
33. Vignesh, S. Endoscopic Diagnosis a me ka maoma o ka pancreatic Cysts / S. Vignesh, W. R. Brugge // J. Clin. Gastroenterol. - 2008. - Vol. 42, N 5. - P. 493506.
34. Ke noho nei i loko o ka maʻi pancreatitis koʻikoʻi: nā hopena o ka mālama mau ʻana ma nā mea maʻi he 76 i nā maʻi / M. Cremer et al. // Endoscopy. - 1991. - Vol. 23. - P. 171-176.
35. Pākuʻi wai transpapillary Endoscopic o ka pseudocysts pancreatic / M. Barthet et al. // Gastrointest. Endosc. - 1995. - Vol. 42. - P. 208-213.
36. Binmoeller, K. F. Endoscopic pseudocyst drainage: kahi hana hou no ka cystenterostomy maʻalahi / K. F. Binmoeller, H. Seifert, N. Soehendra // Gastrointest Endosc. - 1994. - Vol. 40. - P. 112-114.
37. Hoʻopilikia ʻana i nā pseudocysts pancreatic me ka hoʻouluuluʻana o ka wai e ka transpapillary pancreatic duct endoprosthesis / M. F. Catalano et al. // Gastrointest. Endosc. - 1995. - Vol. 42. - P. 214-218.
38. Endoscopic-ultrasound-alakaʻi i ka hoʻokele Endoscopic alika o ka pateudocysts pancreatic a
pupono / C. V. Lopes et al. // Kukulu. J. Gastroenterol. - 2007. - Vol. 42, N 4. - P. 524-529.
39. ʻO ka hana pono o ka hana endoskopiko o ka preudocysts pancreatic / M. E. Smits et al. // Gastrointest. Endosc. - 1995. - Vol. 42. - P. 202-207.
40. Mahele hōʻeuʻi hōʻeuʻeu hōʻike i ka hopena me ka hopena o ka hopena no ka maʻi pancreatic cysts / P. V. Garelik a me nā mea hou aku // Nā pilikia o ka hana ma ke ʻano o ke ʻano o kēia wā: mat. ʻO XIII Congress o nā loiloi o ke Aupuni Repubalika o Belarus. - Gomel, 2006. - T. 1. - S. 92-93.
41. Cuschieri, A. Laparoscopic opra o ka pancreas / A. Cuschieri // J. R. Coll. Nā mea hoʻohālikelike. Edinb. - 1994. - Vol. 39. - P. 178-184.
42. Ke ala, L. Laparoscopic pancreatic cystoga-strostomy: ka hana mua i ka mahele hou o ka hoʻomaʻemaʻe lapalapa palema intraluminal / L. Way, P. Legha, T. Mori // Surg. Endosc. - 1994. - Vol. 8. - P. 240244.
43. Brugge, W. R. hoʻokokoke pili i ka punawai o ka pseudocysts pancreatic / W. R. Brugge // Curr. ʻOlama. Gastroenterol. - 2004. - Vol. 20. - P. 488-492.
44. ʻO ka papa maʻi pancreatic Laparoscopic i nā maʻi me ka maʻi pancreatitis / L. Fernandez-Cruz et al. // Cronic pancreatitis / M. Buechler et al .. -Heidelberg: Blackwell pub., 2002 .-- P. 540-551.
Kūlana no ka leka uila
210023, Republic of Belarus, Vitebsk, pr. 4runze, 27, Vitebsk State Medical University, Keʻena ʻOihana Hoʻolālā, FPK a me PC, tel. kauwa .: 8 (0212) 22-71-94 Schastny A.T.